By Lynne Eldridge, MD Updated on January 17, 2022
Medically reviewed by Doru Paul, MD
You’re likely reading this because you are experiencing what you can only describe as a lung pain, are wondering what’s behind it, and are eager to know how you can improve it.
It’s helpful to first know that the term lung pain is a misnomer. This is because there are no pain receptors in the lungs. And those in the thorax (the chest cavity) provide the brain with only vague information about the precise location of pain.
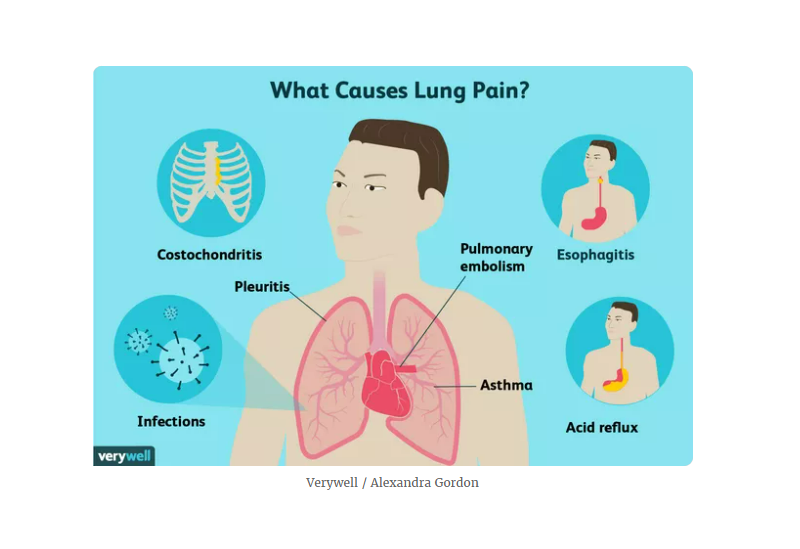
What may seem to be pain in the lungs may be related to asthma or another pulmonary concern. But since several muscles, joints, and organs are located near each other within the chest, your discomfort could instead be the result of something entirely unrelated, such as an inflamed joint, an injured muscle, or more seriously, a diseased heart.
This article explores the triggers of what may be considered lung pain, including pulmonary issues, chest muscle concerns, heart conditions, and esophageal issues. It also explains how a healthcare provider is likely to home in on a diagnosis and how the condition might be treated.
Causes
There are many possible reasons for what may feel like lung pain, some of which may come as a surprise to you.
Pulmonary Issues
Issues involving the lung are a good place to start. These include asthma, infections, and other concerns.
Asthma and COPD
Both asthma and chronic obstructive pulmonary disease (COPD) are respiratory diseases that may be associated with tightness across the chest, especially during a flare or an attack.1
Other symptoms of an asthma attack include a cough that is worse at night, difficulty breathing, and wheezing (a high-pitched whistling sound). Wheezing may also occur in people with COPD, along with shortness of breath, a chronic cough, and sputum (mucus) production.
Infections
Infections ranging from pneumonia and bronchitis to a lung abscess (pus-filled cavities in the lungs) can cause lung pain. Often, an infection in the lung is accompanied by a fever and a deep cough.
Pulmonary Embolism
A pulmonary embolus is a life-threatening cause of lung pain that occurs when a blood clot in the legs called a deep vein thrombosis breaks off and travels to the lungs.
Pain with a pulmonary embolism is sometimes difficult to distinguish from pain due to other causes, although it’s generally sharp. Other symptoms that may occur with a pulmonary embolism include a cough, shortness of breath, a fast heart rate, and calf tenderness, warmth, and swelling.
Pleuritis
Pleuritis refers to an inflammation of the tissues lining the lungs (the pleura). The pain of pleuritis is generally increased with a deep breath and feels sharp rather than dull or achy.
There are multiple health conditions that trigger pleurisy in the lung, including autoimmune diseases, like systemic lupus erythematosus4 and rheumatoid arthritis, as well as bacterial or viral infections of the lung.
Pneumothorax
A pneumothorax (collapsed lung) may cause pain—usually a sudden, sharp chest pain, along with difficulty breathing. In addition, it may be accompanied by crepitus in the chest, a sensation that feels like you have bubble wrap popping under your skin.
A pneumothorax may occur for different reasons. It can happen on its own (seen in people in their 20s with no lung disease) or as a result of an underlying lung disease, like COPD.
Cancer
Cancers including lung cancer and mesothelioma (cancer involving the lining of the lungs) may cause pain, as can non-cancerous lung tumors such as hamartomas.
Lung tumors often cause pain on the same side as the cancer and may be associated with other symptoms, like coughing up blood (hemoptysis) and weight loss.
Pulmonary issues are a common source of lung pain. These issues include asthma and COPD, infections, pulmonary embolism, pleuritis, and pneumothorax. Cancer, and particularly lung cancer and mesothelioma, can also be to blame.
Chest Muscle Pain
People who experience muscle-related pain in their chest area may feel like it’s coming from their lungs.
Costochondritis
Costochondritis is a muscular chest pain syndrome often involving inflammation in the regions where the ribs join the sternum (breastbone). With this condition, people commonly report stinging, gnawing, or sharp areas of pain on the front of their chest.
Fibromyalgia
Fibromyalgia is a central sensitivity syndrome that causes widespread musculoskeletal pain, despite the lack of visible muscle or joint injury or inflammation. Some people with fibromyalgia specifically note tenderness in the chest wall area (tender points), which can be mistaken for lung pain.
Autoimmune Conditions
A few autoimmune conditions may cause pain in the lung area. For instance, some people with rheumatoid arthritis (RA) develop inflammation of the sternoclavicular joint, which connects the collarbone to the breastbone. This causes all-over pain in the front chest area.
Likewise, with ankylosing spondylitis, inflammation of various joints may cause pain in the mid- to upper back and ribcage. This may be erroneously perceived as related to a lung problem.
Chest muscle pain can feel like it’s coming from the lungs. In fact, you could be feeling the effects of costochondritis, fibromyalgia, or an autoimmune condition such as rheumatoid arthritis.
Heart Conditions
Pain in the chest or lung area often raises concern about an underlying heart-related condition. Physicians often suspect angina (chest pain that is caused by coronary artery disease) or a heart attack, when blood flow to a part of the heart is blocked.
Besides pressure, heaviness, or tightness felt in the center or left side of the chest that gets worse with exertion, other potential symptoms of a heart attack include:
- Dizziness and/or passing out
- Nausea and vomiting
- Pain that moves to the neck, jaw, or shoulder
- Palpitations
- Sweating
- Trouble breathing
- Weakness
Other heart conditions may also manifest as lung pain, including:
Aortic Dissection
Your aorta supplies oxygen-rich blood to your tissues and is the largest artery in your body. Aortic dissection causes sudden and severely sharp chest and back pain that can feel like something is ripping inside of you. It is a medical emergency and requires immediate surgical repair of the torn aorta.
Pericarditis
Pericarditis refers to inflammation of the sac that surrounds the heart. It may cause sharp or stabbing chest pain that gets worse while inhaling or coughing. The pain is classically eased by sitting up and leaning forward.
Heart conditions like aortic dissection and pericarditis can cause lung pain. So can a heart attack, so heed the warning signs, which include dizziness, nausea, palpitations, sweating, trouble breathing, and weakness. Call 911 immediately if you suspect you may be having a heart attack.
Esophageal Issues
The esophagus is the hollow tube that carries food and liquid from your mouth to your stomach. Sometimes, conditions that affect the esophagus can cause pain that may be perceived as lung pain.2
Acid Reflux
Acid reflux, or gastroesophageal reflux disease (GERD), is an under-recognized cause of pain that can be felt in the region of the lungs and heart, often behind the breastbone.
The pain is often burning in nature and most commonly occurs after eating. Regurgitation of acid with some undigested foods is also common with GERD.
Esophagitis
The pain of an inflamed esophagus tends to be felt behind the breastbone and is associated with difficulty and/or pain with swallowing. Esophagitis may occur as a result of taking certain medications, receiving radiation, or from infection with a fungus or virus.
Food allergies and a buildup of an immune cell called eosinophils may also cause esophagus inflammation (eosinophilic esophagitis).
Since the burning sensation of acid reflux can be felt in different areas, it’s easy to confuse it with lung pain. Esophagitis is another esophageal condition that can manifest itself as lung pain.
Other Concerns
Sometimes, pain stemming from diseases of your digestive organs, like your gallbladder or pancreas, can spread to the chest.
Pain can also be referred, meaning that it feels like it’s occurring in the chest but really is coming from another region—for example, a herniated disc in your back.
Besides radiating or referred pain, psychological diseases like panic attacks can cause chest pain from hyperventilation. So can shingles (herpes zoster) on the chest or back—a skin condition that causes a burning, blistering rash.
When to See a Healthcare Provider
Although extensive, this list of possible causes of lung pain is not an exhaustive. This is why it’s important to make an appointment to see your healthcare provider, even if you feel there is an obvious reason for your pain.
For example, while chest wall tenderness is a hallmark feature of musculoskeletal chest pain, the presence of tenderness does not exclude a life-threatening cause like a heart attack or a blood clot in the lung.
When to Call 911
Call for emergency medication attention if you experience chest pain that is:
- Severe and/or prolonged
- So bad you feel as though you’re going to pass out
- Associated with symptoms like trouble breathing
Diagnosis
The diagnosis of lung pain begins with a detailed medical history and physical examination.
Medical History
Your healthcare provider will ask you many questions in order to determine the source of your pain. Knowing what to expect can help you prepare:
- How long have you had lung pain?
- Is the pain constant or does it come and go?
- Is the pain sharp or is it vague and achy?
- Is the pain in one spot or do you feel it throughout your chest?
- Does the pain get worse with a deep breath?
- Have you been coughing?
- Do you have a fever?
- Do you have any pain in your legs?
- Have you recently experienced unexplained weight loss?
Your healthcare provider will also inquire about your personal and family medical history, as this can provide clues to your diagnosis. Some related questions may include:
- Do you have any medical conditions, such as heart disease or lung conditions, or autoimmune conditions like rheumatoid arthritis?
- Do you have a family history of any heart or lung problems?
- Do you have a history of smoking?
Physical Examination
During the physical examination, your healthcare provider will talk with you to see how well you are breathing.
Noting your coloring is also an important step. Blue lips and/or nails are worrisome and require immediate medical attention, as they suggest low oxygen delivery throughout your body.
After assessing your overall comfort and breathing status, your healthcare provider will inspect your back and chest wall to look for any rashes or chest and spine deformities.
They will then listen carefully to your lungs and heart sounds with a stethoscope. The provider may also perform an abdominal exam or joint exam if they suspect that the pain could be stemming from a gastrointestinal or rheumatological issue.
Tests and Imaging
Depending on the results of your physical exam, your healthcare provider may order one or more of the following tests or imaging studies:
- Spirometry: This pulmonary function test that measures how much air you can breathe in and out, and how quickly you can empty your lungs. This test is key to diagnosing asthma and COPD.
- Chest X-ray to look for signs of infection
- Blood tests to rule out a heart attack and to look for evidence of inflammation or autoimmune conditions
- Electrocardiogram (ECG), a test to evaluate the heart’s electrical activity, to evaluate for a heart attack
- Stress test: This assesses your heart’s functioning during physical activity, which can aid in the diagnosis of heart disease.
- Echocardiogram: Sound waves produce an image of your heart. This is used to evaluate your heart valves, look for fluid around your heart, or detect heart damage.
Treatment
As you might guess, treatment of perceived lung pain is highly variable and depends on the diagnosis.
For example, if a chest X-ray reveals pneumonia as the culprit behind your pain, your healthcare provider will treat you with one or more antibiotics and tell you to rest and drink fluids. They may also recommend a cough medicine that contains codeine or a nonsteroidal anti-inflammatory drug (NSAID).
For severe cases of pneumonia, or if you are of advanced age, you may require hospitalization for pneumonia treatment.
If angina is the source behind your pain, a heart specialist called a cardiologist can prescribe a medication like a nitrate or beta-blocker. This can relax the blood vessels that travel to the heart and reduce the heart’s workload.
Since heart disease is the “why” behind angina, your healthcare provider will likely treat you with a cholesterol-lowering medication called a statin and aspirin (a blood thinner) as well.
Summary
If you have pain in the lung or chest area at large, see your healthcare provider about it—and be prepared to give them plenty of time to come up with a diagnosis.
They may not need it, but there are many possible causes, including pulmonary issues, chest muscle pain, heart conditions, and esophageal issues.
The diagnosis process can become complicated if the pain is referred, meaning that it feels like it’s occurring in the chest but really is coming from another region. It’s entirely possible that it could take less time to treat chest pain than to pinpoint its root cause.
Original Article – https://www.verywellhealth.com/lung-pain-symptoms-causes-and-diagnosis-2249389#:~:text=Recap,can%20also%20be%20to%20blame.