Climate change will potentially lead to both higher pollen concentrations and longer pollen seasons, causing more people to suffer more health effects from pollen and other allergens.
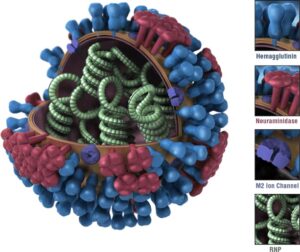
Pollen is an airborne allergen that can affect our health. Pollen grains are tiny “seeds” dispersed from flowering plants, trees, grass, and weeds. The amount and type of pollen in the air depends on the season and geographic region. Though pollen counts are typically higher during the warmer seasons, some plants pollinate year-round.
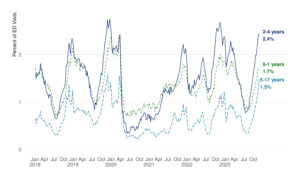
Climate change will potentially lead to shifts in precipitation patterns, more frost-free days, warmer seasonal air temperatures, and more carbon dioxide (CO2) in the atmosphere. These changes can affect:
- when the pollen season starts and ends and how long it lasts each year,
- how much pollen plants create and how much is in the air,
- how pollen affects our health (the “allergenicity” of pollen),
- how much pollen we’re exposed to, and
- our risk of experiencing allergy symptoms.
Pollen exposure can trigger various allergic reactions, including symptoms of hay fever. Hay fever, also known as allergic rhinitis, occurs when allergens like pollen enter your body and your immune system mistakenly identifies them as a threat. If you have allergic rhinitis, your body then responds to the allergen by releasing chemicals that can cause symptoms in the nose. Symptoms of allergic rhinitis can occur during certain seasons or year-round, depending on the allergen, and affect as many as 60 million people per year in the United States. Symptoms from allergic rhinitis include sneezing, runny nose, and congestion.
Pollen exposure can also trigger symptoms of allergic conjunctivitis. Allergic conjunctivitis is the inflammation of the lining of the eye (conjunctiva) due to exposure to allergens like those in pollen. Allergic conjunctivitis is found in up to 30% of the general population and as many as 7 out of 10 of patients with allergic rhinitis. Symptoms from allergic conjunctivitis include red, watery, or itchy eyes.
People with respiratory illnesses like asthma may be more sensitive to pollen. Exposure to pollen has been linked to asthma attacks and increases in hospital admissions for respiratory illness. Medical costs linked with pollen exceed $3 billion every year, with nearly half of those costs being linked to prescription medicine. Higher pollen concentrations and longer pollen seasons can also make you more sensitive to allergens. This can trigger asthma episodes in individuals with asthma and diminish productive work and school days.
Extreme rainfall and rising temperatures also can contribute to indoor air quality problems. For example, they can cause the growth of mold indoors, which may lead to worsened respiratory conditions for people with asthma and/or mold allergies and heightened challenges in maintaining adequate asthma control.
CDC Allergen Resources:
- Asthma – guidance on asthma symptoms, triggers, and management
- Asthma and Allergies in the Workplace – NIOSH resources on a variety of asthma- and allergy-related topics
- Asthma and Mold After a Hurricane – Information for Clinicians Helping Patients with Respiratory Conditions After a Hurricane or Other Tropical Storm
- Covid-19 and Seasonal Allergies – Frequently asked questions about Covid-19 and seasonal allergies
- Pollen and Your Health
Original Article – https://www.cdc.gov/climateandhealth/effects/allergen.htm